While the best treatment for the constellation of abnormalities associated with the restoration of spontaneous circulation is still evolving, ongoing efforts have identified care strategies to improve outcomes. The 2010 American Heart Association (AHA) Guidelines for CPR and ECC contains a useful post-cardiac arrest care algorithm as well as a table documenting a multi-system approach to care, and clear explanations for current recommendations.12 The guideline states: “A comprehensive, structured, multidisciplinary system of care should be implemented in a consistent manner for the treatment of post-cardiac arrest patients.”12
Survivors of out-of-hospital sudden cardiac arrest should have access to a program that includes structured interventions which have been shown to improve survival, including:
- Therapeutic hypothermia
- Hemodynamic stabilization
- Immediate coronary reperfusion when indicated
- Glycemic control
- Neurologic diagnosis, management and prognostication
EMS systems should learn whether the facility to which they transport their patients has the capability to offer these therapies, and whether or not they are implemented when indicated. If a hospital does not, EMS must act in the patient’s best interest to facilitate transport to a facility that does offer the patient the needed system of care. For example, if the post-cardiac arrest 12-lead ECG shows ST-segment elevation myocardial infarction (STEMI), EMS can request air transport to ensure rapid access to a cardiac catheterization facility.
The North Carolina Experience
RACE: Reperfusion of Acute myocardial infarction in Carolina Emergency Departments
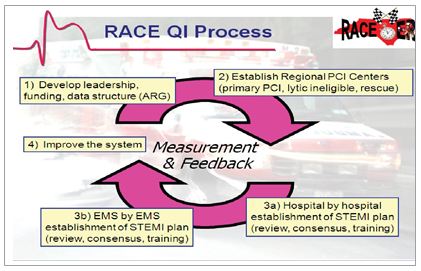
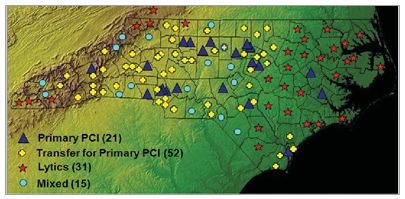
 Since 2003, a dedicated group of medical experts in North Carolina have been collaborating on a project designed to improve rapid coronary artery reperfusion for patients with ST-elevation myocardial infarction (STEMI). The program is called RACE (Reperfusion of Acute myocardial Infarction in Carolina Emergency Departments). The goal of the project was to increase the rate and speed of reperfusion for STEMI patients.
Since 2003, a dedicated group of medical experts in North Carolina have been collaborating on a project designed to improve rapid coronary artery reperfusion for patients with ST-elevation myocardial infarction (STEMI). The program is called RACE (Reperfusion of Acute myocardial Infarction in Carolina Emergency Departments). The goal of the project was to increase the rate and speed of reperfusion for STEMI patients.
The recommendations of this project are based upon established guidelines, published data, and the knowledge and experience of numerous individuals specializing in acute myocardial infarction care.
The RACE statewide system incorporates the quality improvement efforts of 119 hospitals, 540 emergency medical systems, and thousands of healthcare professionals to direct coordinated efforts to provide timely reperfusion. The key elements of the system include regional organization and coordination, institution of the single best plan for treatment at every point of care, ongoing measurement, prompt feedback, and the establishment of teams of healthcare professionals that span all aspects of STEMI care. RACE Website: http://www.nccacc.org/
The success of RACE has been based on the efforts and contributions of hundreds of healthcare professionals across the state of North Carolina. The partnership between the cardiology community and key emergency medicine physicians, nursing leadership through the RACE coordinators and emergency department nurse managers, quality assurance colleagues, and CV administration is critical to the project. The results of the initial RACE project were published in the Journal of the American Medical Association in November 2007, demonstrating substantial improvements in all treatment times across the state.15 The RACE project was named one of the top 10 advances in heart disease by the American Heart Association and is being utilized as a national model for STEMI care.
The RACE Operations Manual was created to guide these systems in implementing the optimal specification by point of care. The manual contains both basic and advanced recommendations that represent features of systems of STEMI care likely to increase the rate and speed of coronary artery reperfusion.
Developing a regional approach to plan for cardiovascular emergencies, stroke, trauma, and pediatric events, begins by assembling experts from all disciplines who are involved in the care of these patients. These discussions should involve local EMS agencies, local hospitals and Emergency Department leadership as well as any state, local or regional representatives that are appropriate (health department leadership, political support — for example the city safety director). Bringing these stakeholders to the table allows dialogue about the importance of regionalized care and a common understanding of current practices.
This wide ranging leadership group can evaluate regional resources and begin to develop standards for the regional care of patients. Working together, a comprehensive plan can be developed to coordinate the delivery of care for victims from the scene of the event, EMS care, destination decisions, communication within the regional system, and feedback on performance of care for these patients. These coordinated efforts will save lives!

